What is Thoracic Outlet Syndrome?
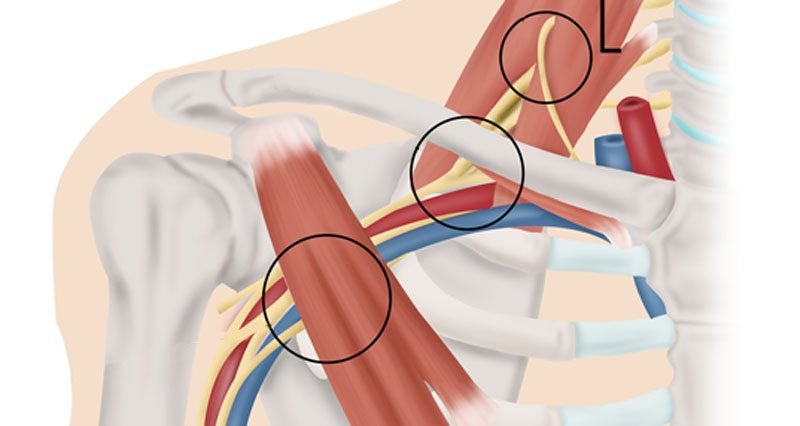
Thoracic Outlet Syndrome (TOS) is a complex condition that arises from the compression of nerves or blood vessels in the thoracic outlet, an anatomical space located between the base of the neck and the shoulder. This area is bordered by the collarbone (clavicle), the first rib, and surrounding muscles, forming a crucial passage through which nerves and blood vessels travel to and from the upper extremities. Understanding the anatomy of the thoracic outlet is essential for appreciating the various presentations of this syndrome.
TOS can present in different forms, primarily categorized into three types: neurogenic, venous, and arterial. Neurogenic TOS is the most common variant, resulting from compression of the brachial plexus, a network of nerves that innervate the arm and hand. Symptoms often include pain, numbness, and weakness in the affected arm. Venous TOS occurs when the subclavian vein is compressed, leading to swelling, discoloration, and pain in the arm. Lastly, arterial TOS is the least common and involves compression of the subclavian artery, potentially causing coldness, paleness, or weakness in the affected limb.
Several factors can contribute to the development of thoracic outlet syndrome, such as anatomical anomalies—like an extra rib—trauma, repetitive activity, or poor posture, particularly in individuals who engage in occupations or activities that require prolonged use of the arms. Recognizing TOS is critical, especially given its impact on the upper extremity and neck. Patients often face challenges in daily activities due to the pain and dysfunction associated with this condition, emphasizing the need for accurate diagnosis and appropriate intervention.
Symptoms of Thoracic Outlet Syndrome
Thoracic Outlet Syndrome (TOS) is characterized by a range of symptoms that may differ based on the specific type of syndrome, which includes neurogenic, venous, and arterial forms. Understanding these symptoms is crucial as they can significantly impact an individual’s daily activities and overall quality of life.
In neurogenic TOS, which is the most prevalent type, symptoms often include pain in the neck and shoulder areas. Patients may also experience numbness and tingling sensations, particularly in the fingers, due to nerve compression. Weakness in hand grip is another common manifestation, which can hinder tasks such as writing or holding objects. These symptoms can impede the ability to perform simple daily activities, leading to difficulties at work or home.
Conversely, venous TOS tends to present with symptoms like swelling in the arm or hand, which may develop quickly. Patients may notice visible distension of veins in the upper limb or experience a feeling of heaviness in the affected area. Such symptoms can interfere with physical activities, causing individuals to alter their routines or avoid certain exercises altogether.
Arterial TOS, although less common, can result in more severe symptoms such as coldness in the hand, pale or bluish skin, and even cramps in the hand or forearm during exertion. These symptoms arise from compromised blood flow and may require immediate medical attention to prevent further complications.
Recognizing these symptoms early is paramount, as timely medical intervention can improve prognosis and enhance quality of life for individuals suffering from TOS. Addressing the symptoms, whether they are neurological, venous, or arterial, through appropriate treatment and lifestyle changes can help mitigate the limitations imposed by the syndrome and promote better health outcomes.
Diagnosis of Thoracic Outlet Syndrome
Diagnosing thoracic outlet syndrome (TOS) can be a complex and multifaceted process due to the condition’s overlapping symptoms with various other disorders. A thorough medical history is critical, as it helps healthcare professionals understand the patient’s symptoms, lifestyle, and any previous injuries or conditions that could contribute to the syndrome. A comprehensive physical examination follows, in which the doctor evaluates the patient’s range of motion, strength, and circulation in the upper extremities.
Several specific tests can be employed to ascertain the presence of thoracic outlet syndrome. Imaging studies, such as magnetic resonance imaging (MRI) and X-rays, are crucial in visualizing structures in the thoracic outlet area. These imaging modalities help identify any anatomical abnormalities, such as cervical ribs or other bony growths that might be compressing nerves or blood vessels. Additionally, ultrasonography may be utilized to assess blood flow and identify vascular issues.
Nerve conduction studies (NCS) and electromyography (EMG) are invaluable in confirming whether there is any nerve damage due to compression associated with TOS. These tests assess the electrical activity of muscles and the speed at which electrical impulses travel through the nerves, thereby helping pinpoint the specific nerves affected by the syndrome. Furthermore, provocative tests, such as the Adson maneuver or Wright’s test, may also be performed to reproduce symptoms and evaluate for the presence of compression symptoms directly.
Despite the array of diagnostic tools available, it’s essential to note the challenges posed by TOS’s symptomatology, which can mimic other conditions such as carpal tunnel syndrome or cervical radiculopathy. Thus, accurate diagnosis is vital for ensuring appropriate treatment strategies are formulated, allowing patients to embark on a tailored therapeutic journey aimed at alleviating their symptoms and improving their quality of life.
Treatment Options for Thoracic Outlet Syndrome
Thoracic Outlet Syndrome (TOS) encompasses a range of treatments, tailored to the severity and underlying causes of the condition. Initially, conservative treatment methods are typically recommended. Physical therapy is one of the primary approaches, focusing on strengthening the muscles around the thoracic outlet, improving posture, and enhancing overall flexibility. Targeted exercises can alleviate symptoms by helping relieve pressure on the nerves and blood vessels. Many patients find relief through consistent sessions with a qualified physical therapist.
Medications also play a crucial role in managing TOS. Nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce pain and swelling, while muscle relaxants may be prescribed to alleviate muscle tension. In cases where symptoms are severe, corticosteroid injections might be indicated to reduce inflammation and decrease nerve irritation, providing temporary relief and complementing physical therapy.
For individuals who do not respond to conservative treatment within a reasonable timeframe, surgical intervention may be considered. Surgical options typically involve decompressing the thoracic outlet, which may include removing a cervical rib or addressing other anatomical abnormalities. Patients should discuss the potential risks and benefits of surgery with their healthcare provider to ensure informed decision-making.
To prevent recurrence after treatment, individuals can adopt certain lifestyle modifications. Maintaining good posture, engaging in regular exercise, and avoiding repetitive overhead activities can significantly reduce the risk of TOS flare-ups. Ergonomic adjustments in the workplace also contribute positively to long-term outcomes. Always consulting with healthcare professionals for personalized recommendations is essential, enhancing the management and prevention strategies for Thoracic Outlet Syndrome.
Disclaimer: This content is for informational purposes only and is not intended to substitute professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified health provider with any questions you may have regarding a medical condition.